L.A. County has fewer than 100 ICU beds available, and the worst is yet to come, officials say

Intensive care unit beds across Southern California are plummeting to critical levels, with capacity falling to 1% in Ventura County and 0% in Riverside County while Los Angeles County — home to 10 million people — had fewer than 100 beds available.
But the worst of the surge is still to come, experts say. L.A. County has more than 4,400 people hospitalized with COVID-19, and officials said that number could rise to 5,000 by the weekend.
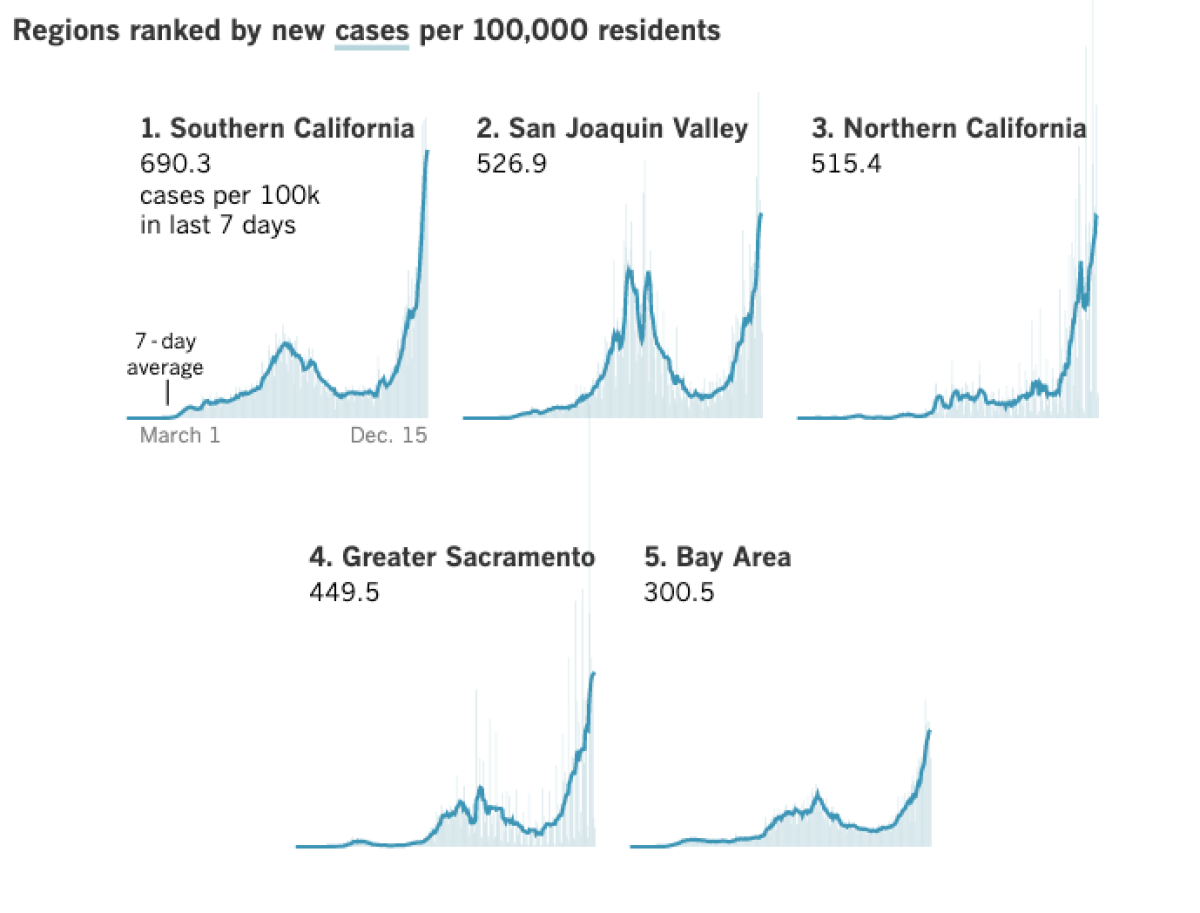
The shortages come as the coronavirus continues to rage across the state. A Los Angeles Times county-by-county tally showed an unprecedented 42,129 cases reported Monday. That number breaks the single-day record set Dec. 8, when 35,400 coronavirus cases were recorded.
“Our reality is frightening at the moment,” L.A. County Public Health Director Barbara Ferrer said.
In L.A. County, COVID-19 hospitalizations are now six times higher than they were in mid-October. On Sunday, there were 935 coronavirus patients in L.A. County’s limited supply of intensive care unit beds — more than quadruple the number from Nov. 1.
In Ventura County, health officer Dr. Robert Levin voiced dismay at people persisting with parties, indoor church services and youth sports events that are currently banned because of the extraordinary public health crisis.
“The numbers are getting to be astronomical. People are going to die that don’t need to die,” Levin said Monday.
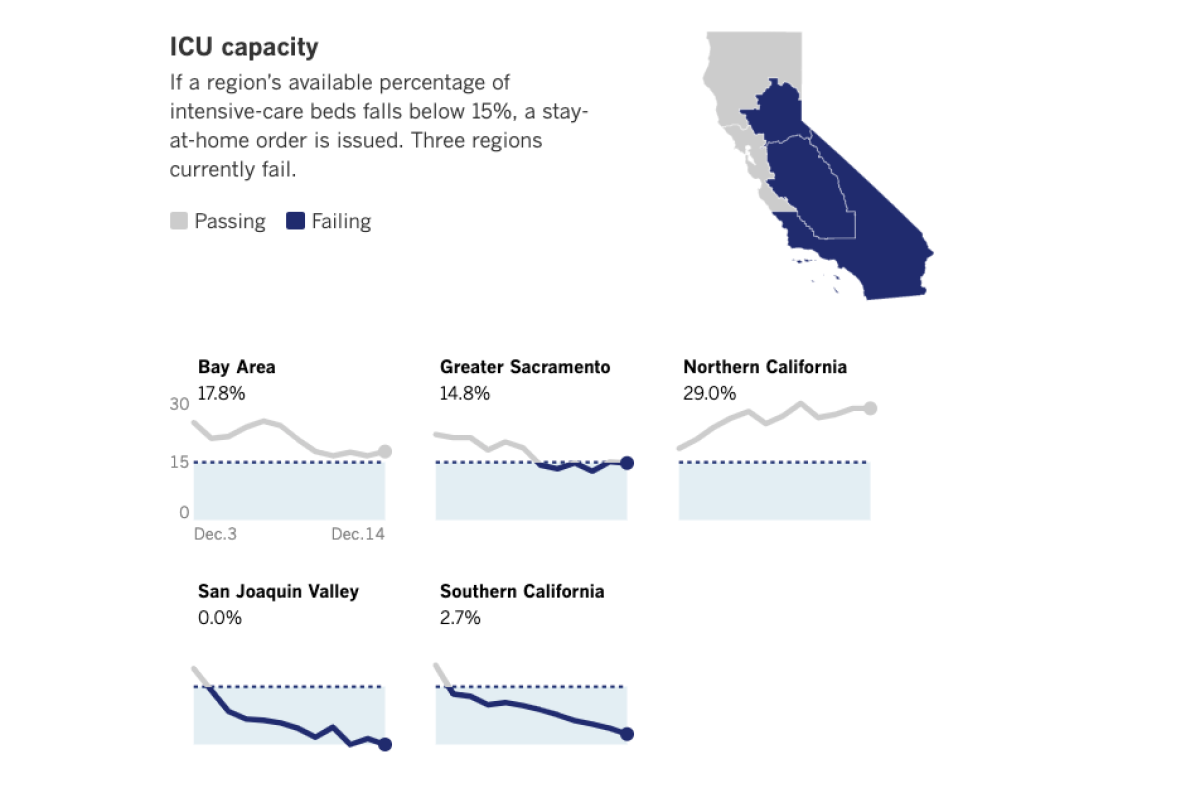
Across Southern California, available ICU capacity fell to 2.7% Monday, down from 4.2% a day earlier. In the San Joaquin Valley, it fell again to 0%, meaning some critically ill patients must be housed in areas of hospitals not normally designed to care for ICU patients, which can increase mortality.
“Many folks may be thinking that this is just not anything to be really worried about because hospitals can just add more beds. The reality is every bed needs to be staffed by highly trained and skilled healthcare workers, and we don’t have an endless supply of healthcare workers, and those that are here saving lives every day are exhausted,” Ferrer said.
“And they’re disheartened by the reality that this isn’t the way it needs to be,” she added. “The best thing that everyone can do right now is stay home as much as possible, and only go out for work, school, exercise or essential services.”
L.A. County is so slammed by COVID-19 patients that for certain periods of time on Sunday, 81% of hospitals who receive patients coming from 911 calls were forced to temporarily divert some ambulance patients elsewhere, said Dr. Christina Ghaly, the L.A. County director of health services.
Ghaly said officials are bracing for hospitalizations to worsen as people infected over Thanksgiving get so sick they need to be admitted. There are roughly 500 new daily COVID-19 hospital admissions in L.A. County, and that number could exceed 700 in a week, Ghaly said.
“We need to brace ourselves that this [hospital] case volume has not yet reached a peak and will keep growing,” Ghaly said.
But while the vaccine offers promise, it comes as the U.S. is facing the darkest moment of the coronavirus crisis. On Monday, the U.S. death toll topped 300,000, and California, like much of the nation, is in the throes of the worst wave of the disease.
Five-hour waits to offload ambulance patients into hospitals
L.A. County is also experiencing the kind of lengthy delays in offloading patients from ambulances into hospitals that Orange County reported last week.
“We’re aware that in certain hospitals across the county, there are prolonged ambulance patient offload times that often do exceed four hours, five hours,” Ghaly said.
As of Monday, L.A. County was averaging nearly 10,700 new coronavirus cases a day over the past week and 58 new COVID-19 deaths a day — both at or near records.
Ferrer said she hoped the stay-at-home order would stabilize or decrease the number of new daily coronavirus cases around Christmas.
Whether that happens depends on whether Angelenos are “actually adhering to this new ‘Safer at Home’ order,” Ferrer said.
Younger adults are spreading the virus the most, Ferrer said, but it’s the oldest adults, when they get infected, who are dying at the highest rates.
“And this is a preventable tragedy because those most vulnerable to serious illness from COVID-19 can be protected by everyone else,” Ferrer said, “when we wear our face coverings, keep our distance, wash hands frequently and avoid mingling with non-household members.”
For years, the faculty of Charles R. Drew University has built trust in South L.A. It’s the best chance of beating hesitancy about the COVID-19 vaccine.
Health officials worry about defiance of health orders
There are concerns about defiance of the orders. After L.A. County ordered a ban on outdoor restaurant dining, the city of Manhattan Beach implemented a plan to allow residents to continue using newly constructed outdoor dining areas as public seating where people can sit and dine out. The L.A. County health officer, Dr. Muntu Davis, has asked the city to “refrain from maintaining a workaround for the temporary suspension of outdoor dining.”
“By placing tables and chairs adjacent to restaurants, the city of Manhattan Beach is both violating and defeating the purpose of the county’s order and decidedly not safeguarding public health,” Davis wrote. The chairs in the newly designated outdoor seating areas match the restaurants’ stock tables and chairs and are not owned by the city, Davis wrote.
The coronavirus case rate in Manhattan Beach has tripled since mid-September, Davis wrote.

In Ventura County, health officer Levin sounded the alarm as COVID-19 hospitalizations there shattered records, breaking the record for 10 consecutive days. On Sunday, 181 coronavirus-infected people were in the county’s hospitals, 72% higher than the peak of the July surge.
Two weekends ago, there were some 80 football players gathered at a park in Simi Valley; sports tournaments are occurring in other counties involving volleyball and baseball players, and in those situations, people weren’t wearing masks, Levin said. Some church services continue to take place indoors, with audience members sometimes sitting shoulder to shoulder, in violation of the rules requiring church services to be held online or outdoors.
The U.S. reached 300,000 fatalities on the same day healthcare workers began receiving Pfizer’s COVID-19 shot.
‘These aren’t just old people that are sick and dying’
At the Oaks mall in Thousand Oaks, there was a report of hundreds of people gathering to sing Christmas carols, many without masks, Levin said. And he’s heard of parties of up to 200 people and residents attending drive-in concerts yet getting out of their cars.
Singing is an extremely high-risk activity and has been documented to spread the coronavirus. One choir practice left dozens infected with the coronavirus and two people dead in Washington state.
“What’s understandable about this?” Levin said at a news conference. “None of these justifications are acceptable in the face of the pandemic. We all need to be working together, just like we would be fighting any war.
“It’s incomprehensible to me. It’s baffling. It’s also irresponsible,” Levin said. “COVID is running so rampant in our county that 1 out of every 10 COVID tests that we run are positive.
“It’s too easy to run into someone with COVID nowadays and not know you’re being exposed,” he said. There are now 49 outbreaks at long-term care facilities in Ventura County.
Levin said one of his daughters works at a hospital in Sacramento. “She told me, ‘Daddy, I look around the hospital: These aren’t just old people that are sick and dying. These are young people, like me.’ It’s heartbreaking. And she’s right.”
The latest maps and charts on the spread of COVID-19 in Los Angeles County, including cases, deaths, closures and restrictions.
‘We’ve had to tell family ... that their loved ones are not coming home’
One of the long-term consequences suffered by some younger people who are infected is the so-called ‘long-hauler’ syndrome, in which survivors can suffer from persistent shortness of breath and a “foggy head” — an ongoing state of confusion and clouded thinking that can persist for months, Levin said.
“Some of these people were joggers. We don’t know if that’s going to be permanent or not,” Levin said. “If we all work together, came together —and I mean figuratively, spiritually, that is — for just three or four weeks, our infections would go away. They would plummet. And our businesses could open.”
Dr. Mark Lepore, an intensive care unit physician at Ventura County Medical Center, said he expects Ventura County to exceed hospital capacity, “and what exceeding capacity looks like is showing up to the hospital and not having a room to go into or not having a staff member to take care of you.”
“The hardest part about caring for COVID ... it’s the lack of families being able to see their loved ones, and it’s horrible to watch,” Lepore said. “It’s how slow and insidious the COVID is that it hits the body. You have symptoms for the first eight or so days, and then you just don’t recover.”
Maybe the fever goes away, but the shortness of breath can last until the end. “We’ve had to tell family members that their loved ones are not coming home, and it’s awful,” Lepore said.
Lepore urged people to avoid gathering for Christmas: “Just tell them you’ll see them next Christmas. This is that important: We don’t want your family members to get sick and not be able to get care.”
Five healthcare workers at Kaiser Permanente Los Angeles Medical Center are among the first in the state to receive a COVID-19 vaccine.
Governor defends stay-at-home order
Gov. Gavin Newsom on Monday said there are some initial signs that the new stay-at-home order — in effect for most of the state for a week — was starting to work to reduce the movement of Californians.
“That is buying us time,” Newsom said.
The governor made the remarks on the same day healthcare workers in Hollywood were among the first Californians to receive the COVID-19 vaccine. Although the news was greeted with optimism, the vaccine comes too late to prevent infection among people who were exposed to the virus over the Thanksgiving holiday.
Amid complaints about the economic burden of the stay-at-home order, Newsom and other officials have defended it as a prudent way to safeguard lives and the economy once the vaccine has been distributed widely.
COVID-19 vaccines are now being administered to healthcare workers in the U.S. What are your questions about the timeline, the safety or the science?
“As soon as this pandemic is behind us, this state will recover more resilient, more vibrant than ever,” Newsom said Monday. “And so the most important thing we can do, from an economic perspective, is focus on public health. Focus on mitigating the spread of this virus.”
UCLA economists last week issued an optimistic forecast, predicting the U.S. economy will experience “a gloomy COVID winter and an exuberant vaccine spring,” followed by robust growth for some years.
Newsom and health officials have defended California’s approach to the pandemic as one that has saved lives. Among the 50 states, the District of Columbia and Puerto Rico, California has the 39th highest cumulative number of coronavirus cases per 100,000 residents and 39th highest cumulative number of COVID-19 deaths per 100,000 residents.
Times staff writers Sean Greene and Margot Roosevelt contributed to this report.
More to Read
Start your day right
Sign up for Essential California for news, features and recommendations from the L.A. Times and beyond in your inbox six days a week.
You may occasionally receive promotional content from the Los Angeles Times.